Long Island Neuroendocrine Dysfunction Lawyer
Law Office of Cohen & Jaffe, LLP.
Between 2000 to 2011, approximately 233,425 military service members reported mild traumatic brain injuries (TBIs). This number occurs during a time when the rate of civilians with mild traumatic brain injuries (TBIs) is reaching 2.5 million. Consequently, approximately 5.3 million Americans are facing long term disabilities due to traumatic brain injuries.
Many of these brain injury victims also face neuroendocrine disorder. This article reviews not just why the neuroendocrine system plays an important role in the human body, but also how injuries can end up disrupting the system’s functions.
The Role of the Neurological and Endocrine Systems
Our neurological system contains our central nervous system, which performs the critical task of regulating bodily functions through the brain and spinal cord. This system also includes the peripheral nervous system, which includes the nerves that perform voluntary and involuntary actions.
The endocrine system contains glands that produce and release hormones into our bodies. These hormones are responsible for controlling basic body functions, which include tasks like bone and tissue growth and heart regulation. Imbalances of hormones occur when a person’s glands produce too much, not enough, or a total absence of one or several hormones.
The neuroendocrine system includes cells located throughout the body. These cells are similar to nerve cells or neurons. These resemble endocrine cells that create hormones. These cells receive signals from the neurological system that develop and release hormones. Neuroendocrine cells can be found in the ovaries, testicles, lungs, gastrointestinal tract, kidneys, liver, skin, and thyroid. These cells also comprise the majority of the pituitary glands, parathyroid glands, and adrenal medulla, which is the inner layer of the adrenal glands.
What Is Neuroendocrine Dysfunction
Neuroendocrine dysfunction refers to various conditions caused by an imbalance in hormone production connected to a person’s brain. Two parts of a person’s brain (the hypothalamus and the pituitary gland) are responsible for regulating hormone production. Damage to these areas as the result of a traumatic brain injury like brain swelling, a rupture, or vascular damage can end up impacting the body’s production of pituitary hormones as well as other neuroendocrine functions.
While neuroendocrine abnormalities are often the result of traumatic brain injuries, they can also be caused by mild brain injuries like concussion. These abnormalities can also sometimes occur following a brain infection like meningitis. Because tumors are a common occurrence in the neuroendocrine system, they must be ruled out before bioidentical hormone therapy or another form of treatment occurs.
Many neuroendocrine dysfunctions occur because hormone levels are either too high or too low. Sometimes, the human body does not properly respond to hormones. When the body experiences an endocrine disorder, the symptoms might present as neurological problems. This is one of the reasons why the assistance of a knowledgeable medical professional is often critical in recognizing neuroendocrine dysfunctions.
Neuroendocrine Dysfunction Symptoms
Many symptoms can occur as a result of neuroendocrine dysfunction, but some of the most common neuroendocrine dysfunction symptoms include:
- Depression and mood swings
- Diabetes
- Fatigue or insomnia
- Headaches
- High blood pressure
- Loss of libido
- Memory loss or altered mental states
- Muscle weakness
As a result of neuroendocrine disorders, some women end up experiencing irregular menstrual periods while men might end up facing erectile dysfunction. In both men and women, neuroendocrine disorder can end up impacting fertility. The more promptly that the neuroendocrine dysfunction is diagnosed and treated, the more promptly that hormone balance can be regained.
The Nature of Traumatic Brain Injuries
In 1918, the first case of post-head trauma hypopituitarism (PHTH) was reported. The syndrome, however, did not receive substantial attention until the turn of the century. Since then, an extensive amount of research has shown the causes and consequences of post-head trauma hypopituitarism, which can include everything from minor injuries to blast-related injuries in veterans.
Unfortunately, anatomic and physiologic complexities of both the hypothalamus and pituitary gland increase their susceptibility to becoming injured as the result of a traumatic brain injury. The pituitary gland is located in a bone pocket referred to as the sella turcica and is covered by a layer of dura matter referred to as the diaphragma sellae. A small but vital organ, the pituitary is approximately the size of a pea and often weighs less than a gram. The pituitary gland is connected to the hypothalamus by a blood vessel-containing stalk. This connection places the pituitary gland (particularly its anterior portion) at great risk of being damaged due to a head injury.
The hypothalamus secretes thyrotropin-releasing hormones and luteinizing-releasing hormones that stimulate or suppress the production of anterior pituitary gland hormones. This stimulation, in turn, results in the release of hormones and other substances from target organs.
How Neuroendocrine Disorders Can Impact Individuals
Neuroendocrine dysfunction caused by traumatic brain injury can interfere with the normal production and regulation of hormones created by both the pituitary gland and the hypothalamus.
The most common hormonal deficiencies associated with traumatic brain injuries include:
- Adrenocorticotropic hormone deficiency. This condition is the result of decreased or absent production of adrenocorticotropic hormone by the pituitary gland.
- Gonadotropin deficiency (LH/FSH/testosterone/estradiol). This condition involves the absence or decreased production of two distinct hormones affecting the reproductive system. Luteinizing hormone stimulates the testes in men and ovaries in women. This deficiency can impact fertility in men and women as well as women’s menstruation. Follicle-stimulating hormone (FSH) can also be impacted as a result of this deficiency.
- Pituitary deficiencies (TSH/FSH/GH/IGF-1) This condition is characterized by the shortage or absence of several hormones produced by the pituitary gland. Lack of any one or a combination of these hormones can impact the development of many body parts.
- Prolactin deficiency. This condition is characterized by the inability of pituitary lactotrophs to secrete prolactin and by the resulting lack of puerperal alactogenesis.
- Thyroid deficiency. The thyroid helps the body to convert food into energy and heat as well as regulate body temperature. An absence or deficiency of thyroid hormone in the body can impact many bodily functions. Thyroid hormone exists in two primary forms: (1) thyroxine (T4) which is an inactive form that is produced by the thyroid gland and converted to T3 in other areas of the body, and (2) Triiodothyronine (T3) which is the active form of T4.
The Effects of Hormone Deficiencies
When a person’s body is short on hormones, there are various ways in which a person’s body can be impacted.
Consider the following types of hormone deficiencies:
- Antidiuretic hormone deficiency caused by TBIs. This can result in excessive urination, dehydration, excessive thirst, and hypernatremia.
- Corticosteroid deficiency caused by TBIs. This condition can result in hypoglycemia, hyponatremia, myopathy, anemia, depression, fatigue, anxiety, weight loss, and loss of libido.
- Gonadotropin deficiency caused by TBIs. Known to result in signs and symptoms like infertility, decreased libido, erectile dysfunction, decreased muscle mass, decreased exercise tolerance, anemia, and testicular atrophy. In females, this deficiency results in amenorrhea, sexual dysfunction, and breast atrophy.
- Growth hormone deficiency caused by TBIs. This condition is most commonly recognized by signs and symptoms like increased abdominal fat, fatigue, decreased concentration, dyslipidemia, anxiety, depression, and impaired judgment.
- Prolactin deficiency caused by TBIs. This can result in decreased libido and impotence in males. In women, this can lead to amenorrhea, galactorrhea, infertility, hot flashes, and vaginal dryness.
- Thyroid hormone deficiency caused by TBs. This is known to cause decreased energy, depression, cold intolerance, weight gain, fatigue, poor memory, muscle cramps, constipation, hypotension, and changes in a person’s hair, skin, and voice.
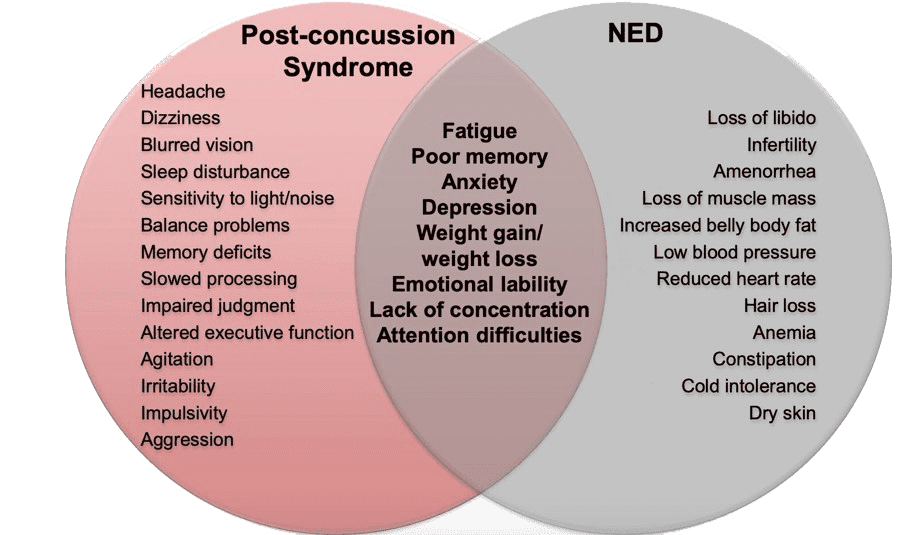
As you might have noticed reading through these descriptions, many neuroendocrine dysfunction symptoms overlap with conditions consistent with post-concussion syndrome.
The Challenges Faced by TBI Victims
Many times, traumatic brain injury victims are either not screened or tested for neuroendocrine disorder with any frequency. Unfortunately, delays in diagnosis or the treatment of Neuroendocrine Dysfunction can also impair a person’s overall recovery and rehabilitation from a traumatic brain injury.
Various sources recommend that any traumatic brain injury victim with persistent symptoms that suggest Neuroendocrine Dysfunction and that do not resolve in three months following the injury or those cases with an onset of new symptoms suggesting Neuroendocrine Abnormalities as far as three years after an injury is sustained be tested for Neuroendocrine Dysfunction. Despite this recommendation, in most places, screening for Neuroendocrine Dysfunction is not occurring despite the many traumatic brain injury victims with persistent post-concussion symptoms.
A recent study published in January 2020 by the Journal of Neurotrauma reviews and analyzes research addressing the prevalence of Neuroendocrine Disorder. This study found that approximately “one-third of TBI sufferers have persistent anterior pituitary dysfunction 12 months or more following trauma”.
Insurance carriers do their best to minimize the necessity for testing, screening for, and treating neuroendocrine abnormalities. Unfortunately, however, it is often an issue of cost for insurance carriers in addressing the condition. Consequently, these companies often put their profits over the importance of properly treating TBI victims. For example, a deficiency in GH can end up resulting in up to $20,000.00 a year for supplemental hormone injections.
Speak with an Experienced Long Island Personal Injury Lawyer
Neuroendocrine Abnormalities can leave people facing numerous consequences. If another party was responsible for causing an accident that led to these injuries, it is important to remember that you have the right to pursue compensation.
Contact Law Office of Cohen & Jaffe, LLP today to schedule a free case evaluation.